Each time you go to a brand new physician, you do the identical factor: Fill out lengthy varieties with all of your insurance coverage info, then give your insurance coverage card to the receptionist. So what occurs subsequent within the insurance coverage course of? How does a declare undergo as soon as the cardboard is within the fingers of the physician’s workplace?
Let’s begin with a easy definition. A medical health insurance declare is a invoice for well being care companies that your well being care supplier turns in to the insurance coverage firm for cost. With many plans, if you go to the physician for a routine checkup and your invoice is $100, you pay a co-pay or coinsurance of $25 and your physician payments your insurance coverage service for the remaining $75.
Your insurance coverage declare truly begins earlier than you even make an appointment. Your insurance coverage service is accountable just for paying advantages which can be lined beneath your coverage, so it’s best to perform some research to keep away from being shocked if you settle up along with your physician or pharmacist. Do not hesitate to ask your insurance coverage consultant to make clear something you do not perceive. Learn your coverage totally so you realize what’s lined. That is particularly essential when one thing comes up, like a prognosis that requires therapy not lined in your coverage.
After you’ve got paid, your physician sends your invoice to an insurance coverage claims processing heart. The processing heart gathers all related info out of your physician — the affected person info sheet, consumption varieties and the right companies documentation. These are in comparison with the insurer’s clarification of advantages to see if the coverage covers the companies. If it does, your insurance coverage service will submit cost for the remaining steadiness. If not, you’re liable for no matter steadiness is left after your co-pay.
That sounds simple sufficient, does not it? Most claims processes are easy, however you could encounter some bumps within the highway — the dreaded denied claims. We’ll discover out what to do about these within the subsequent part.
Denied Well being Insurance coverage Claims
“”
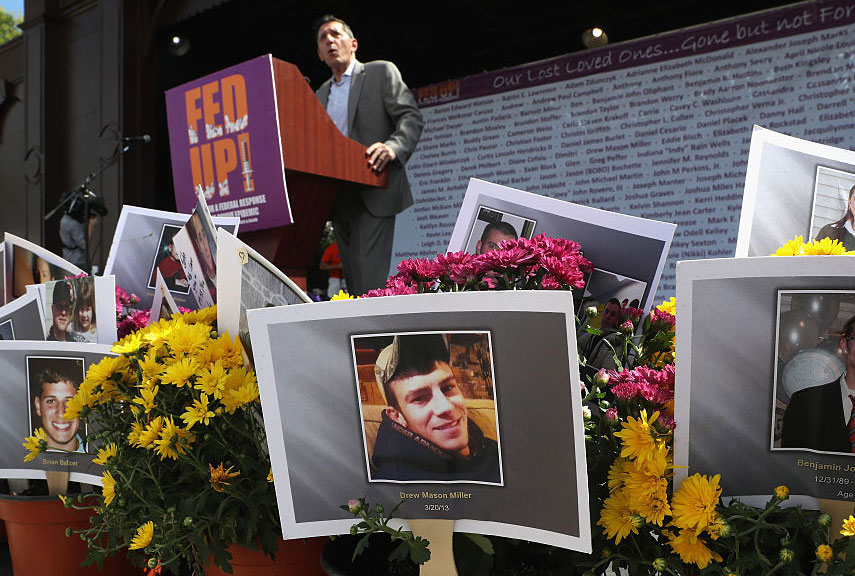
You probably have a denied declare,you’ll be able to request a proper evaluationby the insurance coverage firm.
Stockbyte/Getty Pictures
So, your declare has been denied, and there is a enormous invoice ready to be paid. Claims could be rejected as a result of the plan does not cowl the process, treatment or provide, or as a result of the insurance coverage firm deems it medically pointless or experimental. When you suppose you’ve got taken all of the measures to keep away from a rejected declare — like calling the insurance coverage firm earlier than the go to or totally reviewing your coverage — you’ll be able to try to flip the denial to acceptance.
If a declare is denied for any motive, together with administrative error on the a part of the insurance coverage firm, a fast cellphone name might clear up the issue. If this does not work, you’ll be able to request a proper evaluation by the insurance coverage supplier. You will need to resubmit your declare, which is reviewed by a well being care skilled who specializes within the area during which the process or treatment belongs.
We should word right here that you just normally must undergo with these formal critiques inside a strict time line. In case your formal request is denied, there may be yet another effort that might repay. Every state has its personal division of insurance coverage that works to make sure that customers are protected and that the regulatory processes of the insurance coverage corporations are honest. So, a name to your state’s insurance coverage division may assist.
For extra details about medical health insurance claims, try the hyperlinks on the subsequent web page.
Frequent Causes for Denied Claims
- Remedy sought with out prior authorization
- Improper declare submitting (lacking info, illegibility)
- Claims not filed inside deadlines
- Remedy not lined by coverage
- Process deemed medically pointless
Learn Extra