Utilization assessment is a well being insurance coverage firm’s alternative to assessment a request for medical remedy. The aim of the assessment is to verify that the plan offers protection for your medical providers. It additionally helps the corporate reduce prices and decide if the advisable remedy is suitable. A utilization assessment additionally offers you the chance to verify that your well being plan offers enough protection on your specific situation. If the corporate denies protection because of a utilization assessment, you’ll be able to at all times attraction the choice.
The time period "utilization administration" is usually used interchangeably with utilization assessment. Though they each contain the assessment of care based mostly on medical necessity, utilization administration normally refers to requests for approval of future medical wants, whereas utilization assessment refers to opinions of previous medical remedy. So, utilization administration is the method of preauthorization for medical service. You can even use it for approval for added remedies when you’re present process medical care (a concurrent assessment). Evaluations of appeals additionally fall below utilization administration.
The time period "utilization assessment" refers to a retrospective assessment — the assessment of remedies or providers which have already been administered, and assessment of medical recordsdata as compared with remedy pointers. Within the latter case, info retrieved throughout a utilization assessment can be utilized as a part of a system that creates the insurance coverage firm’s pointers for a given situation. When creating these paperwork, insurance coverage corporations not solely use affected person experiences but in addition assessment how physicians, labs and hospitals deal with the care of their sufferers.
On this article, we’ll dig deeper into the forms of utilization opinions and administration and discover out what to do in case your assessment is denied. Let’s begin with precertification opinions.
Precertification Evaluation
Precertification is the preapproval course of for remedies discovered in your insurance coverage coverage’s precertification listing. The size of the listing varies by plan sort, however most lists embody nonemergency hospitalizations, outpatient surgical procedure, expert nursing and rehabilitation providers, house care providers and a few house medical tools. The assessment and approval entails figuring out whether or not the requested service is medically mandatory.
Most insurance policy have predetermined standards or medical pointers of take care of a given situation. So, when you submit a precertification request to an insurance coverage firm, a committee opinions these pointers and determines when you’ve got met the standards for precertification protection. If mandatory, the committee might contact your well being care supplier. The overall course of for precertification is comparable in most well being care plans.
The method begins with the gathering of data, together with the signs, analysis, outcomes of any lab assessments and listing of required providers. The committee then opinions the standards on your situation. It might examine your medical info to the well being plan’s medical necessity standards. If the committee denies your request, you can begin the appeals course of.
Subsequent we’ll go over concurrent and retroactive opinions.
Kinds of Utilization Evaluations
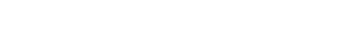
“”
A medical health insurance firm, hospital or unbiased group can conduct a retrospective assessment.
Photographer: Endostock | Company: Dreamstime
Very similar to precertification opinions, concurrent opinions are used for approval of medically mandatory remedies or providers. Nonetheless, concurrent opinions occur throughout energetic administration of a situation, be it inpatient or ongoing outpatient care. The main target of concurrent assessment is to make sure that the affected person is getting the suitable care in a well timed and cost-effective method.
This course of is very similar to that of precertification. After you start a medical remedy, any new remedies discovered on the insurance coverage firm’s preapproval listing are submitted to the insurance coverage firm for approval. Info on the care you’ve got acquired, alongside together with your present medical standing and any progress you’ve got skilled, is collected. As soon as the insurance coverage firm or an unbiased assessment group opinions the data, the doctor and different suppliers are notified with the choice.
An necessary a part of concurrent assessment is the evaluation of the affected person’s wants after a hospitalization. As a result of concurrent assessment is used to lower the period of time you spend within the hospital, the primary concurrent assessment typically determines a discharge plan. This plan can embody transfers to rehabilitation, hospice or nursing services. Whereas discharge plans typically change as a result of issues or irregular take a look at outcomes, establishing an early timeframe for hospitalization is essential to retaining medical health insurance prices down.
So what occurs when you did not get preapproval however bought the medical care anyway? That is the place retrospective opinions are available.
The retrospective assessment entails the assessment of medical information after your medical remedy. The insurance coverage firm can use the outcomes to approve or deny protection you will have already acquired, and the data will also be utilized in a assessment of the insurance coverage firm’s protection pointers and standards for a specific situation. The insurance coverage firm appears by way of your information for proof of applicable low-cost well being care. It then compares your information to these of different sufferers with the identical situation. It’ll then assessment, and presumably revise, its remedy pointers and standards to make sure that the offered care is enough, and medically present, for the situation. This primary sort of retrospective assessment might be carried out by the medical health insurance firm, an unbiased assessment group or the hospital concerned within the remedy.
The opposite perform of retrospective assessment is the approval of remedies that usually require precertification however had been completed with out approval. This will occur if a affected person is unresponsive and has not been capable of receive precertification. Emergency providers like surgical procedure additionally could also be eligible for this sort of assessment. The assessment takes place earlier than any fee is made to the supplier or hospital. Subsequently, most hospitals or suppliers are actively concerned within the assessment course of by offering medical documentation that helps their remedy selections.
What occurs when a utilization assessment is denied? We’ll clarify the appeals course of within the subsequent part.
Maintaining it Honest: State Requirements for Evaluations
When processing precertification and concurrent opinions, well being care corporations should abide by requirements established by state legislatures. These requirements are quite a few, however most states embody the next:
- Affected person info needs to be restricted to that wanted for the assessment carried out.
- Choices should be made in a well timed method.
- All events should be notified of assessment selections.
- The standards used to find out medical necessity should be clear.
- An appeals course of should be established.
- The assessment workers needs to be appropriately credentialed.
Learn Extra
The Appeals Course of
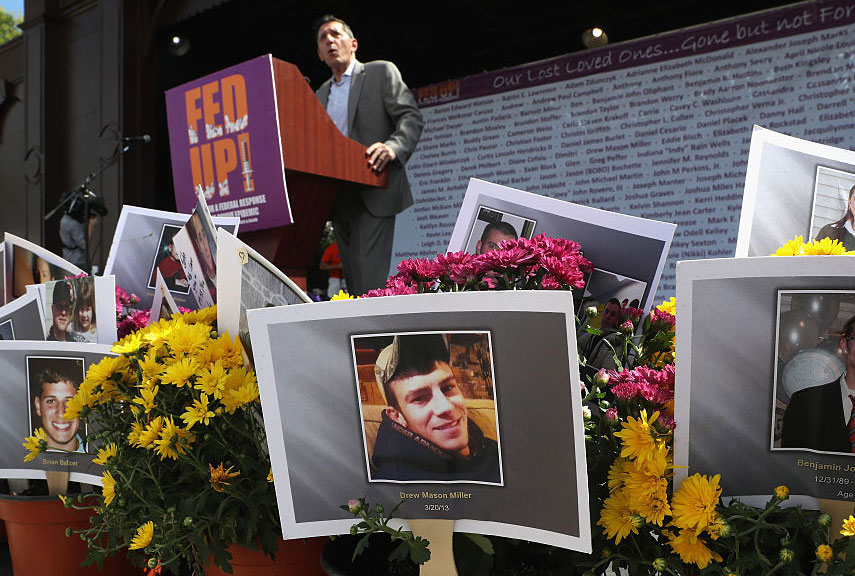
“”
Medical doctors who’re registered utilization assessment brokers can decide in your attraction.
Photographer: Gelpi | Company: Dreamstime
The appeals course of begins after your insurance coverage firm offers you an "hostile willpower" letter. This letter should come inside three days of the preliminary utilization assessment and should embody the explanations your request was denied, info on how this denial might be appealed and knowledge on methods to receive the corporate’s medical assessment standards. As soon as you’ve got acquired this letter, you will have the choice to file an attraction.
Step one could also be apparent — name your insurance coverage firm to say you wish to file an attraction. If you happen to depart a message with this info, the insurance coverage firm is required to return your name inside one enterprise day. At this level you’ll be able to select an expedited or commonplace assessment of the attraction. Usually, you’d need an expedited assessment when the denied medical protection is required instantly. Decide the usual assessment when you do not want the protection instantly or if an expedited assessment is denied.
As soon as the attraction begins, you or your supplier might have to supply the insurance coverage firm with extra medical info. This info needs to be reviewed by the insurance coverage firm or outsourced to a utilization assessment group. Licensed and registered utilization assessment brokers (normally physicians or different well being care suppliers) who find out about your specific situation should make this resolution.
After you’ve got handed over all of the requested info, the insurance coverage firm should reply to your attraction inside a set timeframe. For expedited appeals, it’s best to obtain a call inside two enterprise days. With an ordinary attraction, the choice needs to be issued inside 60 days. These time frames can show extraordinarily necessary — in case your plan doesn’t reply throughout the set time line, the preliminary denial of protection is robotically reversed and your insurance coverage firm should pay for the providers. So you should definitely preserve monitor of what you despatched and while you despatched it.
In case your attraction is denied, your insurance coverage firm is required to ship you a "last hostile willpower" letter. This doc ought to embody the precise causes for the denial, together with any mandatory medical explanations. It must also present info on how one can obtain a duplicate of the insurance coverage firm’s medical assessment standards. Lastly, relying in your state’s legal guidelines, the letter might embody info on methods to make an exterior attraction that entails a third-party decision-maker, normally an unbiased assessment group.
For extra details about utilization opinions, check out the hyperlinks on the subsequent web page.
What’s an Impartial Evaluation Group?
Impartial assessment organizations (IROs) assessment quite a few medical subjects, like workman’s comp and experimental remedy opinions. They’re generally utilized in utilization opinions, working as third-party mitigators between medical health insurance corporations and sufferers. Medical insurance corporations can use IROs to ascertain remedy pointers and standards, and so they will also be introduced in when an attraction of an hostile utilization assessment has been denied. On this function, they act as each affected person advocates and as advocates for cost-effective well being care, which serves in the perfect curiosity of the medical health insurance corporations.